Disclaimer: There may be affiliate links, which means I’ll receive a commission if you sign up for a free trial or purchase through the links, but there is no extra cost to you.
Elbow pain: Do you know what is Medial Epicondylitis?
Medial epicondylitis, also known as a golfer’s elbow, is much less common than lateral epicondylitis (tennis elbow), but it is the most common cause of pain in the inner elbow.
It is a type of inflammation that occurs in the flexor tendons of the forearm. For you to better understand: the arm bone, called the humerus, has two bumps or lumps in the region near the elbow. These protuberances are called medial and lateral epicondyles. Medial epicondylitis, as its name implies, is the inflammation of the tendons of the medial epicondyle.
The “golfer’s elbow” pain can appear suddenly or gradually and is characterized by:
- Pain and tenderness on the inside of the elbow;
- Possible weakness in the hands and wrists;
- The elbow can become stiff and hurt when you close your wrist;
- Numbness or tingling that radiates to one or more fingers, usually the ring and pinky (About 50% of cases of medial elbow epicondylalgia have neurological symptoms associated with compression of the cubital nerve);
- There may also be pain when you close your hand with your fingers inward;
- The area can be extremely sensitive to touch and pain can radiate from the forearm.
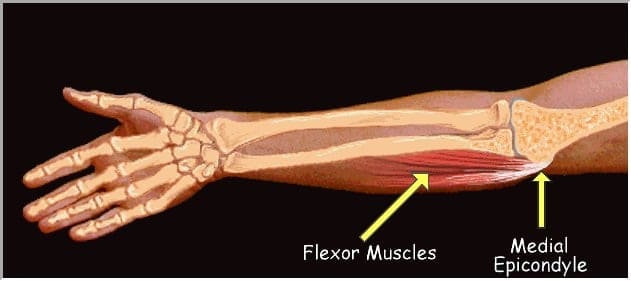
These tendons are responsible for those flexing movements that we are used to doing every day, such as flexing the fingers, bending the wrists and turning the palm down, for example.
Medial epicondylitis is also known by the informal name of “golfer’s elbow” because due to the movements required in this activity, the incidence in the practitioners of the sport is quite large. Medial epicondylitis occurs in about 0.5% of the general population, mainly in people between the ages of 45 and 55 who are active.
An elbow pain with a very similar name is lateral epicondylitis , which would be the “tennis player’s elbow”. In this case, the pain is more concentrated in the lateral region of the elbow, due to the arm extension movements performed during tennis games and other physical and sports activities
What are the causes and symptoms of medial epicondylitis
Medial epicondylitis can have several causes. The repetitive overload on the local tendons is one of the main reasons. Sports such as golf, weight training and tennis cause this overload several times during physical activity and can cause this type of epicondylitis.
Activities that require repetitive efforts in this area also create the problem. Another very common cause is trauma in the region by blows, knocks and accidents, which can injure muscles and tendons.
The symptoms of medial epicondylitis are easy to observe, so its diagnosis is also usually quick. When medial epicondylitis appears, the affected person feels acute pain on the inside of the elbow, just where the medial epicondyle is. Pain or discomfort can radiate throughout the forearm, but on closer inspection, it will still have its most painful spot near the medial bone in the elbow.
It is usually possible to diagnose medial epicondylitis with clinical examination and observation of the patient’s symptoms. Ultrasound and even MRI may be necessary when the patient does not respond to initial treatments, doubts in the diagnosis or if there is a need to exclude the presence of other associated lesions.
How to make the diagnosis of medial epicondylitis?
The diagnosis of medial epicondylitis can usually be made on the basis of a physical examination. If a person has medial epicondylitis, the pain is usually felt in the elbow.
Golfer’s elbow patients usually experience pain and tenderness in the inner elbow. Lifting, carrying and even shaking hands can cause a sharp pain that can radiate from the elbow to the wrist. Throwing athletes may experience pain during the throwing movement and prolonged pain after activity.
Physical examination findings include local tenderness over the medial epicondyle, and pain with flexion of the resisted wrist or pronation of the forearm. An increase in pain in the medial epicondyle with resisted isometric flexion, repetitive flexion and pronation of the wrist can also be assessed.
Some patients will show signs of compression of the ulnar nerve at the elbow with tenderness over the ulnar nerve or numbness and tingling in the ring and small fingers, known as cubital tunnel syndrome.
Imaging exams
The diagnosis of a golfer’s elbow can usually be made only with physical examination and medical history, but imaging of the elbow can be useful in particular cases.
Radiographs generally do not show lesions, unless the chronicity of the condition has allowed the development of periostitis in the affected epicondyle
Magnetic resonance imaging or ultrasound can be used to diagnose medial epicondylitis and assess the severity of the disease.
If symptoms of the ulnar nerve are present, electroencephalography or nerve conduction tests may be performed to assess cubical tunnel syndrome.
Complications of medial epicondylitis
In addition, medial epicondylitis may also be associated with other problems, such as ulnar nerve neuropathy. A compression of this nerve, also known as the cubital tunnel syndrome, which is located just after the medial epicondyle. It usually tingles the fingers, especially between the fourth and fifth fingers. In more severe cases it can cause loss of strength in the region.
The disease can also be associated with medial instability of the elbow. It tends to occur mainly in those who practice sports activities frequently, such as throwing, which requires repetitive valgus movement and can cause injuries to the medial ligaments of the athlete’s elbow.
Sometimes, medial epicondylitis can result in a complication. It is the involvement of the ulnar nerve because the proximity to it is great. This nerve is precisely the one that causes us a sensation of shock when we hit the elbow on an object or piece of furniture.
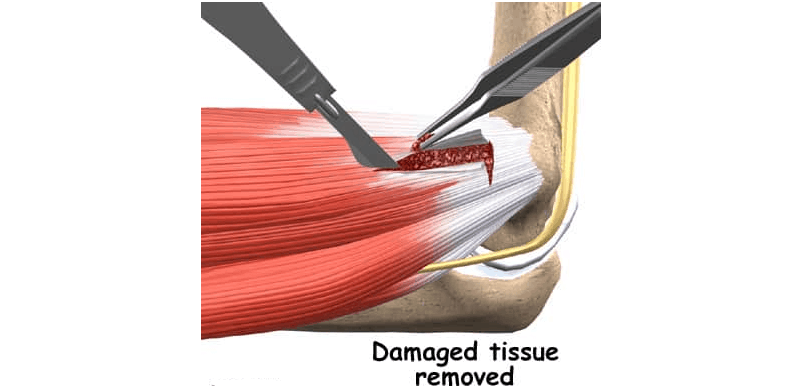
The patient who had medial epicondylitis if he presents frequent tingling in the hand, especially in the ring and little fingers, possibly has a problem with the ulnar nerve. In this case, new physical exams must be done to assess the need for surgery where a tendon debridement (cleaning) and nerve decompression are performed.
How is the treatment of medial epicondylitis

The treatment of medial epicondylitis is based on three important factors: pain control, rehabilitation of the musculature that has been reached and prevention to reduce the risks of the problem occurring again.
Usually the treatment achieves the desired results and has a success rate that varies between 88% to 96% depending on the case. This will depend on the causes, the chosen treatment and also the patient’s commitment to do what the doctor asks.
Pain control can be achieved in several ways.
The main forms are therapies such as physiotherapy and acupuncture , performed alone or in combination.
In addition, experts indicate the use of anti-inflammatory medications that can be oral or topical, immobilization of the affected area and orthoses. To choose the best curative method, the doctor takes into account not only the profile of the case but also the patient’s health history.
Sometimes infiltrations can be indicated, usually when other previous treatments used are not effective, but as they present some risks, they must be discussed between doctors and patient and are not usually performed routinely.

In parallel, the causes of medial epicondylitis are evaluated in order to avoid the activities that caused it, whether at work, at home or in sports activities. In this way, the problem is worsened and the chances of rehabilitation treatment are increased.
Rehabilitation begins after recovery from the acute painful phase. To rehabilitate the tendons of the medial epicondyle, a series of exercises is recommended based on stretching the flexor muscles, with the activation of the antagonistic muscles for the result to be more effective. The exercises also aim at strengthening the muscles. Rehabilitation is achieved in a simple way, but its total evolution can take up to a year depending on the case. Strengthening the region can also be achieved with acupuncture and physical therapy.
A new option for these cases is shockwave therapy , which has shown good results in the treatment of several musculoskeletal disorders , such as medial and lateral epicondylitis , plantar fasciitis , myofascial pain syndrome and other pains.
Often, the pain of medial epicondylitis ends up resulting in a nociceptive increase, that is, other associated pains appear due to disuse and musculoskeletal contractures, such as myofascial pain. Thus, an effective treatment can be done with the combination of pharmacological treatment + acupuncture + infiltrations + physiotherapy.

Prevention should be done to prevent the problem from returning and pain relapse. It mainly takes into account the causes of the emergence of medial epicondylitis. For those who are athletes, for example, there is an assessment and adequacy of both the technique used in sports activities and the sports material used to practice the sport.
Since medial epicondylitis occurs due to the overuse of the muscles that flex the wrist, it is important not to overload them. At the first signs of pain on the inside of the elbow, one should decrease the activity and seek medical attention. The pain of a “golfer’s elbow” doesn’t have to keep you off the field or away from your favorite activities. With rest and proper treatment, you can return to a normal life.
When surgery is needed for medial epicondylitis
When all this pain relief, rehabilitation and prevention treatment does not reach the expected result, surgery may be necessary. It is a very rare situation because generally the measures taken for rehabilitation, when performed correctly, usually resolve. However, there are few and few cases that need surgery!
Surgery requires some prior exams. Its purpose is to remove diseased tissues. If there is any change in the ulnar nerve, it must also be treated. The most common is decompression of the cubital tunnel region. This nerve can be transferred, that is, transposed to an anterior region below or above the forearm muscles. Surgery can be done by anthroscopy or open route.
And how is the diagnosis made?
Anyway, when it comes to rheumatoid arthritis, as well as other autoimmune diseases, it is essential that the diagnosis is made early, after all, it is the best way to manage to live with the pathology, which is chronic and has no cure.
The perception of the main symptoms should be a reason for attention and in case of persistence of them for a minimum period of six weeks, it is necessary to resort to medical support.
Only from the clinical examination, in association with laboratory tests, is it possible to be sure of the presence of the pathology, the level of the clinical condition and to know how to act to minimize the damage.
In addition, we reinforce that in view of the discovery at the beginning of the disease, well-being and quality of life are maintained. It is enough for the patient to follow simple guidelines from qualified health professionals to provide them.
Finally, we remember that for having a lower risk of developing the disease, it is ideal: maintaining healthy eating habits, exercising, sleeping well, controlling weight and not smoking.

